
Major Health Insurer Modernizes Contact Center Operations with Voice AI
Phased transformation powered by Kore.ai improves efficiency, enables agent assist, and lays the foundation for agentic AI.
reduced
post-call documentation
improved
multilingual accuracy
up to 40%
lower operational costs
Healthcare
10,000+
United States

Overview
A large North American healthcare payer that serves millions of members across diverse multilingual communities faced rising call volumes and too much manual documentation. This put pressure on agents and made it harder to deliver fast, consistent service.
The payer partnered with Kore.ai to modernize operations and improve member experiences using AI for Service, starting with AI-powered automation and expanding into transcription, summarization, and intelligent agent assistance. This progressive rollout is improving service quality, lowering operational effort, and positioning the payer for a more agentic member service model.
The Challenge
The large payer's contact center manages high call volumes across English and Spanish-speaking member populations. Repetitive inquiries and manual documentation workflows added pressure on agents, increasing handle times and creating inconsistent member experiences. Rising expectations for speed and accuracy made it difficult to maintain efficiency at scale.
Key pain points included:
- High volumes of routine inquiries that diverted agents from more complex member needs
- Manual documentation steps that extended post-call workload and lengthened handle times
- Transcript accuracy challenges across multilingual channels, creating downstream inefficiencies
- Limited real-time support for member service representatives, increasing the effort required during complex calls
The Solution
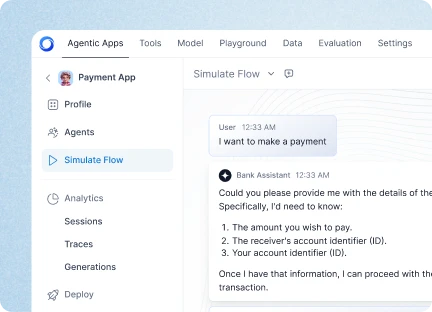
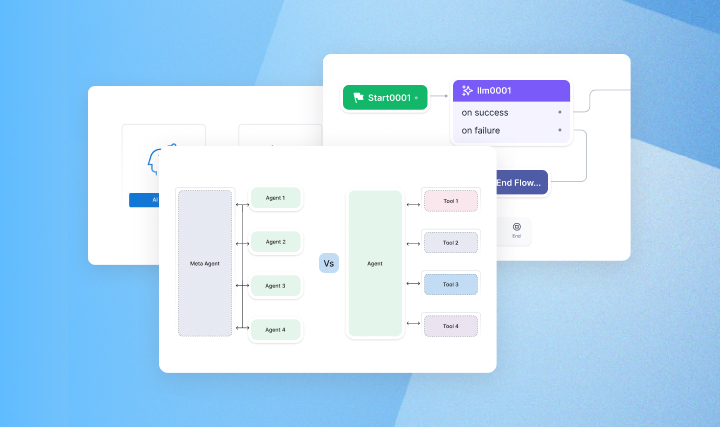
The payer introduced a phased implementation of AI for Service, using Kore.ai to modernize its member services organization and accelerate its shift toward a more agentic operating model. The initiative began by easing demand on member service representatives through front-end automation and has expanded into AI-powered transcription, summarization, and intelligent agent assistance to elevate service quality and improve operational efficiency.
Phase 1 introduced an AI-driven front-end experience for both voice and digital, where AI Agents handled common inquiries and routed members more efficiently. This contained routine demand and reduced the workload on member service representatives.
Phase 2 introduced AI-powered transcription and summarization, automatically capturing key details from member interactions and reducing post-call documentation time. Kore.ai’s partnership with Deepgram provided the transcript accuracy needed across the payer's multilingual population, enabling consistent summaries and improved efficiency.
Phase 3 added real-time intelligent agent assistance, enabling AI to support member service representatives with contextual suggestions and recommended next steps. This enhanced consistency across interactions, reduced handle times, and strengthened the member experience.
Together, these phased enhancements establish a strong foundation for the payer's ongoing transformation toward a more agentic, AI-enabled member services organization.
Business Impact
The payer's phased implementation of AI for Service is delivering measurable gains across member experience, operational efficiency, and support team performance. These improvements directly address the organization’s earlier challenges of rising call volumes, multilingual demand, manual documentation burdens, and the need to better support member service representatives during complex interactions.
Key Outcomes:
- Higher containment of routine inquiries as AI Agents now resolve high-volume, repeatable requests, easing pressure on member service representatives
- Significant reduction in post-call documentation time through AI-powered transcription and summarization
- Improved multilingual accuracy and consistency, strengthening downstream processes and record quality
- More effective support for member service representatives through real-time intelligent assistance
- Meaningful cost efficiencies, putting the payer on a strong trajectory toward achieving up to 40 percent lower operational costs
- Together, these outcomes show how the payer's phased adoption of AI for Service is strengthening efficiency, elevating member interactions, and moving the organization toward a more agentic, AI-enabled service model.
The Kore.ai Advantage
Kore.ai provides the payer with an enterprise-grade foundation built for the scale, complexity, and regulatory demands of healthcare. AI for Service enables automation of high-volume interactions, real-time intelligent assistance for member service representatives, and accurate summarization of call details, all while maintaining strong compliance and security aligned with healthcare standards. Kore.ai helps the payer modernize its operations responsibly, and provides a model other healthcare organizations can follow as they elevate member experience and improve performance.








.webp)